Health Care Assignment: Case Study Analysis for Palliative Care Of A Patient
Question
Task:
Palliative care is for people of all ages with a life limiting or life -threatening condition. WHO defines palliative care as ‘an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.
A life-limiting condition is a condition for which there is no reasonable hope of cure, from which the person is expected to die. Some of these conditions cause progressive deterioration rendering the person increasingly dependent on family and carers. A life-threatening condition is usually of short duration with an acute or unexpected onset. Curative treatment may be feasible but can fail. It may or may not occur in the context of a pre-existing life-limiting condition.
The case study in this assignment enables you to analyse and discuss palliative care in the context of the individual, whanau/family and from a M?ori perspective.
Case Study for Palliative Care Assessment
Meet Mrs. Smith
Mrs. Smith, a 71-year-old female, was admitted to the hospital with an exacerbation of her chronic obstructive pulmonary disease (COPD) and pneumonia. Her symptoms were cough, fever, headache, and shortness of breath. Mrs. Smith also had a history of diabetes and was in the hospital with pneumonia three weeks prior.
Over the next few days, Mrs. Smith's condition worsened. She was transferred to the intensive care unit (ICU) when the infection spread to other organs of her body, inducing shock. Her care was transferred to the on-call resident who was unfamiliar with her case. She continued to complain of headache and shortness of breath, and the nurses noted that she was increasingly irritable and hardly slept. During the night, Mrs. Smith suffered an acute nosebleed and aspirated blood into her lungs, causing respiratory distress, and she was intubated. Once an independent woman, Mrs. Smith now lay in the ICU with a spreading infection and a ventilator pumping air into her lungs to keep her alive.
Mrs. Smith's son and daughter-in-law came to visit every afternoon. They noticed a significant change in Mrs. Smith's health status and spirit but remained hopeful that she was “a fighter”, and would turn around. By writing on a pad of paper, Mrs. Smith communicated to her son that she was very uncomfortable and particularly worried about missing Sunday Mass. As Mrs. Smith's condition continued to decline, she became confused and disoriented. She did not have an advance health care directive, and when the doctor initiated a discussion about her code status, the family was uncertain of what to do because they had never discussed it before. The family did not understand why her condition was not improving and became increasingly worried about the cost of the hospital stay.
The case of Mrs. Smith presents several concerns:
- First, Mrs. Smith failed to receive adequate pain and symptom management-she continued to be short of breath while her headache and insomnia were completely overlooked.
- Second, inadequate communication between the patient, family, and clinical team meant that goals of care were not discussed while Mrs. Smith was still able to communicate, and the family never realized the severity of Mrs. Smith's condition.
- This led to uncoordinated care that compromised Mrs. Smith's quality of life and her autonomy when decisions needed to be made.
- Mrs. Smith received suboptimal care that failed to meet her physical, psychosocial, and spiritual needs.
Read the case study carefully and prepare a detailed health care assignment responding to the following.
Part 1:
Analysis
In the context of the case study.
- Consider physical, psychological, social, spiritual, and cultural needs to analyse how lifethreatening illness has affected Mrs Smith.
- Analyse the impact life-threatening illnesses have, in general, on whanau/family. You can write about emotional challenges, financial problems, social isolation, stress, and burnout.
Part 2:
Critically discuss
Dying people may experience a range of symptoms including, but not limited to, pain, nausea, vomiting, constipation, excessive secretions, breathlessness, agitation, and restlessness. It is the health professionals` role to use their knowledge and skill to assess, plan, implement, monitor, and reassess the patient and the effectiveness of interventions to relieve and control symptoms.
Effective communication and patient advocacy are fundamental to achieving a sound symptom control treatment plan.
- Drawing from the case study, critically discuss how effectively Mrs Smith’s pain and other distressing symptoms were handled by the palliative care team.
- From holistic point of view, discuss how important the health professional’s role is in providing symptom control?
- Critically discuss how emotional and spiritual healing be provided as part of palliative care?
Part 3:
Examine the health professional’s role
M?ori life expectancy is improving, and an increasing number are 65 years of age and older. However, the combination of high rates of life-limiting disease and an increasing aged population suggests that M?ori access to palliative care should also be increasing.
- Examine the role of health professionals in responding to M?ori individuals with life threatening diseases, including their whanau/family.
- Analyse the importance of health literacy and communication for health professionals when providing palliative care for Maori individuals, whanau/family?
- Discuss significant M?ori beliefs and traditions that can influence health professionals’ decisions when providing care and services?
Answer
Introduction
The following health care assignment sheds light on the case of Palliative care which can be defined as the approach centered on the patients so that care can be taken for advancement in disease so that they can put focus on the quality of life and the relief of the symptoms of the patients. Palliative care should be provided to the patients according to their individual needs. For this analysis, a case study was considered which involved a 71-year-old Mrs. Smith afflicted with multiple diseases that have affected her well-being and put her in need of palliative care. According to Etkind et al. (2017), the need for palliative care will increase in the next decades, and the rise in chronic illnesses may be responsible for the rise in cases requiring palliative care. The Mãori perspective will be especially considered for investigation in this report focusing on a particular demographic segment.
Part 1
Analysis
Evaluation of how life-threatening disease has affected Mrs. Smith
The physical needs of Mrs. Smith were raised due to the illness that she was suffering from. As a patient of palliative care, she was faced with multiple physical problems, which included her requiring treatment and care for her illness, which was chronic obstructive pulmonary disease and the infection being spread across her body. She required professional attention for better management of the pain and symptoms that she had due to her illness. She was suffering from various physical issues, which caused her to not be able to perform the tasks properly, which may have caused her stress that aggravated her conditions. The disease can bring disorders like pain, fatigue, and disorders with the mood that she was keeping. She required constant monitoring of her conditions and care that aligned with her needs (Mithrason & Parasuraman 2017). She also had been suffering from diabetes and had been afflicted by pneumonia three weeks before being admitted due to chronic obstructive pulmonary disease. This must have rendered her weak due to the constant encounters with multiple life-threatening illnesses.
As the illness progressed, the healthcare staff members saw her irritability increasing since the illness was probably making her stressed and tired, and insomnia that she was suffering from could be contributing to this. The physical imbalance and the turmoil that she had to go through physically contributed to the stress. The cognitive functioning and the way in which she performed her tasks were impaired (Conversano 2019), and this may have caused emotional stress. The diagnosis of the disease may have caused grief in her, making her irritable due to the overwhelming feelings and a deteriorating view of her own body image. Uncertainty about the future may have led to the individuals being more affected by the disease.
Social needs of having a family around, the quality of her life, the connections with society, financial security and stability affected by the medical costs, need for counseling regarding the physical activity and dietary conditions, and professional care regarding the behavioral issues that she was exhibiting (Tong et al. 2018). Along with the diagnostic labeling and technical solutions from the healthcare professionals, according to Ming et al. (2019), she needed ethical behavior, which included compassion in their attitudes, effective and professional communication, respect of the rights that she had as a patient, and providing a satisfactory quality of care which could have helped in building the relations between her and the nurses that looked after her, which would be her social needs.
The spiritual needs of Mrs. Smith were also affected by the life-threatening illness that she was going through. The spiritual needs would include an emphasis on the present conditions that she was living in, which might help in neutralizing the effects of the uncertainty that was brought by the illnesses. The stress and anxiety could be reduced in this way for Mrs. Smith. Spiritual assistance could help her connect with herself and thus be able to negate the self-esteem issues that she could be facing due to the long-term illnesses. According to Astrow et al. (2018), unmet spiritual needs like not being able to make sense of the illness that she was afflicted with could have been an issue with Mrs. Smith. She also was confused about not being able to attend her religious and spiritual commitments, which may have affected her morale during the period of the disease that she was dealing with.
Her adherence to the therapeutic regime that she was subjected to by the hospital that she was admitted to could have led to her cultural beliefs being affected and her viewing the illness from her cultural lenses. The cultural beliefs that she had needed to be respected, and she needs the healthcare staff to be culturally competent to be able to have personalized care that can align with her linguistic and cultural requirements. The cultural needs require the patient to be educated regarding her illness in a way that she can understand and provide care with sensitivity towards her ethnic and cultural orientation (Shahin, Kennedy & Stupans 2019). The basic needs of Mrs. Smith are to make them feel more connected, with continuous care, the feeling of cultural sensitivity, and a sense of belonging in the community. The cultural needs of Mrs. Smith were not attended to properly at the hospital.
Implications of Life-Threatening Diseases on Family
The family of Mrs. Smith was affected by the illness that she went through in many ways as well. They had concerns regarding their finances because medical costs are high, and thus these may cause the families to have to face problems. The homeostasis of the family was disturbed by this illness of Mrs. Smith. The illness made the family have to face disturbing emotions, which led to stress and anxiety and fostered feelings of helplessness. Unmet needs of the family could lead to distress in the family and thus compromise the recovery process of the patient as well as the quality of life of the family members themselves (Damanik & Chen 2021). Families usually want to be involved in the care of their patients and derive emotional satisfaction from that usually. They also have to face issues with being in psychological distress, with uncertainty in the prognosis of the patients that could develop from the lack of connection with the healthcare professionals taking care of their patients, and face challenges with the visitation policies (Greenberg et al. 2021).
The families of the life-threatening patients could be faced with challenges like financial hardship, isolation, depression, being challenged physically and emotionally, poor time management, being deprived of sleep, and inadequacy of their privacy. There is a lack of support for the caregivers in the family to be able to adapt to the current situation and their development of anxiety, stress, and depression (Keramatikerman 2020).
Financial hardships could lead to debts for the family, which can lead to further stress in the family members. The debts can cause mental and physical health issues for the family members of the patient. The son and daughter-in-law of Mrs. Smith, for example, we're worried about the costs of the hospital, and this may have forced them to reduce the quality of healthcare being provided to Mrs. Smith by the professionals due to unaffordability.
The partner of the patient would have to provide support to the patient while also looking after their own needs caused due to stress from the partner being ill. This can cause tiredness and fatigue, along with emotional drainage and problems with the balance between the extent to which the patient is dependent or autonomous about their needs. Parents who have children with life-threatening illnesses also have to face challenges regarding their own well-being, which include communication issues with their spouses, an increase in possibilities of divorce in the families, and strain in the roles that the parents have to play in the caregiving position. The constant caregiving process can give way to possibilities of burnout in the palliative care of the patients since the families could be tired from the constant responsibilities and fatigue in the caregiving role that they were playing.
Part 2
Critical Discussion
Drawing from the case study, critically discuss how effectively Mrs. Smith's pain and other distressing symptoms were handled by the palliative care team.
Pain and symptom management can be deemed as the most important parts of palliative care for patients. Along with the support for the patients with regard to their spiritual, psychological, and social beings, the management of the patients requires the management of the symptoms that they have been exhibiting with proactiveness. According to Altilio et al. (2019), the lack of control over the pain and symptoms can influence the experience of not only the patient but also the staff members, the family, and so on. The pharmacological management of pain mainly involves opioids, but safety is imperative in the prescription of these medications since they are highly abusable. The symptoms like pain, anxiety, breathlessness, fatigue, as we're being shown by Mrs. Smith, were mostly ignored by the healthcare staff at the hospital, which may have led to the aggravation of the symptoms due to inadequate presence of prompt action for the care of the patient. While the irritability of the patient was taken into account, it was not acted upon by the nurses in the healthcare facility, which reduced the quality of life for the patients. The patient, as well as the whanau, can face multiple dimensions of pain, including affective, sensory, and cognitive pain. The healthcare organization failed to provide Mrs. Smith with the pain management strategy that she needed due to them neglecting to formulate one that suited her.
Effective communication is one of the most important factors that lead to effectively finding ways in which the symptoms can be managed. Communication between the patient and the healthcare professional needs to be transparent so that the professional has a clear idea about the needs of the patient and thus can organize the strategies around the needs of the patient. The issue with Mrs. Smith was that she had had prior encounters with medical issues, and after she was transferred to the intensive care unit, she had to have her case handled by an on-call resident who was not aware of her medical history properly. This leaves room for issues in the treatment due to her not being able to connect with the professional attending to her, which may be detrimental to her treatment. Her health spirit was seen to have been deteriorating thereafter with issues rising about the condition of her health. She complained about her headaches and breathlessness and had irritability and insomnia. The lack of effective communication may have led to the deterioration of her condition in this situation. The symptoms could be controlled by the proactive approach taken by a healthcare professional (Baillie et al., 2018). Caring for people who are suffering from life-threatening conditions has many challenges to the action, which include the identification of the patients who are the most vulnerable to the threats posed by the illnesses, identifying their issues and using multidisciplinary medical fields in order to ensure that their problems are addressed without them being subjected to many risks, making sure that the patient is communicated with for understanding their needs, besides the needs outlined by the technical diagnostic tests so that their needs are attended to the best.
Figure 1: The WHO Pain Ladder
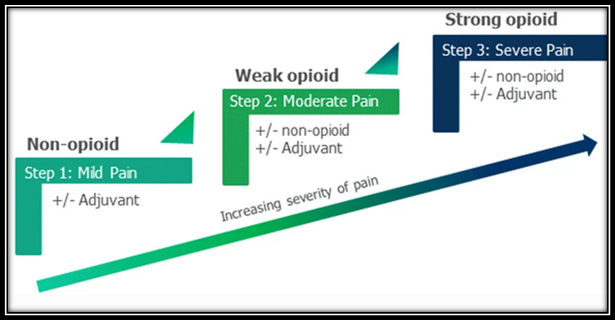
(Source: Dißmann et al. 2018)
Figure 1 shows how the WHO Pain Ladder prescribes different analgesics for different levels of the severity of pain. This can be used as guidance for effectively managing pain and ensuring all patients are the recipient of suitable reliefs for their pain and could have been used for Mrs. Smith.
From a holistic point of view, discuss how important the health professional's role is in providing symptom control.
Health professionals are involved in the engagement of the patients in patient-centered care and special palliative care that can help in increasing the quality of life that the patients get from the organizations. The professionals perform the assessment and the treatment of the symptoms of the patients, which can contribute to making decisions and coordinating the treatment of the patients throughout the period of the disease. General practitioners or family physicians can also help since they can provide the most well-allocated resources for the patients due to their familiarity with the case of the patient, and this can help in the communication and coordination with the other professionals in the medical field when needed. The nurses are essential workers since they can provide critical support and advice, with control over the nurse-patient relationship that contributes to the way in which these patients are handled. Physiotherapists and occupational therapists can support the patients in the domestic environment so that they can improve the quality of life for the patients. Psychologists and other mental health professionals can help in providing help following the behavioral, social, and emotional factors of palliative care, which means that they help in supporting the patients through the period of their illnesses. The grief counselors can help the families in being able to manage their grief in case of a tragic consequence, which can also help the patient if required for addressing their needs. There are other professionals for providing emergency medical support, for providing spiritual and mental support to the patients and their families so that they can have their quality of life improved in navigating the life-threatening illness. The healthcare professionals are responsible for providing help in the diagnosis, treatment, and response to the illness that they have been encountering for palliative care (Hahn 2020). Even music therapists contribute to palliative care by helping the patients calm down and understand their spiritual connections better. Music therapy has been found to reduce pain in the patients and contribute to improvement in the quality of life of the patients. The functioning of the patients has been observed to improve, and their psychological issues addressed in this manner so that they can have better access to care in the organizations (Gao et al., 2019).
Critically discuss how emotional and spiritual healing be provided as part of palliative care.
Collaborating with the chaplains can help with the emotional and spiritual needs of the patients to be met easily so that they are able to heal emotionally and spiritually. These collaborations can also help the healthcare teams and the families of the patients in being able to avail of spiritual and emotional well-being during the disease continuum (Ruth-Sahd, Hauck & Sahd-Brown 2018).
Focus group meetings, according to Asadzandi (2018), were conducted to find that the psychological and physical well-being of the patients were also dependent on the kind of counseling and self-care that they indulged in and can contribute to the increase in the sense of trust that they have on higher powers spiritually, which can help in being able to foster the emergence of security in the family and the healthcare systems and be able to deal with the other patients. Focus group meetings can also provide the emotional healing that can be provided to them with the emotional instability, tension, and uncertainty being alleviated for the patients and their families. It is important to provide the patients with the delivery of spiritually integrated and flexible cognitive behavioral therapy that can help the patients in being able to receive entitled spiritual psychotherapy that can help with their treatment in palliative care. The validation of the struggles that the patients are going through can be essential for their treatment so that they are healed spiritually and emotionally (Rosmarin et al., 2019). Treatment that is centered on the patients can provide them with the best care that can be suited to their requirements.
Part 3
Role of the Health Professional
Role of the Health Professionals in Response to the Mãori individuals with life-threatening diseases, with their family
The health professionals are responsible for providing the patients with the care that is best suited to their conditions and make decisions regarding the goals of the care and the way to achieve the goals of the treatment by providing coordinated care that can help in improving the quality of life for the patients as well as their families, with optimized care for the psychosocial, physical, and spiritual requirements of the patients. This way, the healthcare professionals would be able to understand the requirements of the patients and would be able to foster the patient advocacy and effective communication required for the control of the symptoms in the patients.
Palliative care is delivered to the Mãori individuals with a focus on the way in which they are oriented in relation to the geographic, cultural, and health policies that they belong to. Since the current care-of Mãori individuals are more inclined towards the Western culture, there is a need for the health professionals to be more culturally competent and diverse in the way in which they address the issues of the different patients that they need to cater to. Cultural nuances around health, injuries, and deaths need to be known to the healthcare organizations so that they are able to contribute to the patients being able to access the most suited healthcare practices. Stereotypes can cause healthcare professionals to provide discriminatory treatment to the Mãori individuals.
The health professionals can help the healthcare organizations in being able to provide them with compassionate care for the individuals, with respect towards the autonomy of the individuals in making decisions for their treatment and care.
Importance of health literacy and communication for health professionals when providing palliative care for Maori individuals, whanau/family
Health literacy refers to the ability of an individual to be able to access, interpret, and utilize information obtained about healthcare services. According to Brooks et al. (2020), the healthcare professionals would need to engage in health literacy for the betterment of the quality of palliative care that they can provide to the Mãori individuals. Healthcare literacy screening tools like Test of Functional Health Literacy in Adults, Newest Vital Sign, Rapid Estimate of Adult Literacy in Medicine, and so on can help in the health literacy of the professionals to be assessed so that they are able to use this for caring for their patients. Healthcare professionals can be prone to low self-esteem if their health literacy is low, and so they should develop their literacy to be able to be more confident regarding the health information being used. Healthcare professionals need to engage with the patients and their families with effective communication skills so that there are no misunderstandings regarding the treatment methods. The main issues that are related to the misunderstandings among the patients and the healthcare services include the cultural differences regarding the aspects like relations with authority, perceptions of spirituality, issues with physical contact, the styles of communication, and the sexuality, gender, and family in the culture of the patient.
Healthcare professionals would need to help the patients by being engaged in motivating the patients to participate in their treatments, by encouraging them to be asking the right questions, identifying and formulating the problem, setting the goals and milestones for their treatment, choosing between the options for management, and exercising control over the ways in which medical interventions are being used in the treatment of the Mãori individuals.
M?ori beliefs and traditions that can influence health professionals’ decisions when providing care and services
Cultural values and traditions of the Mãori community can influence the decisions of health professionals when they engage in palliative care. The Mãori views on healthcare are based on four main elements, which include the wairua (spiritual), whãnau (extended family), hinengaro (psychological), and tinana (physical). For the improvement of the Mãori health status and bringing more equity in the healthcare services, there is a need to address the diverse requirements of the different individuals in the community (Capital & Coast District Health Board 2022). The framework for the Mãori healthcare services is the Te Whare Tapa Wha, which has the four cornerstones that define the Mãori health parameters, which are psychological, spiritual, familial, and physical factors (Best Practice Advocacy Centre New Zealand 2022). Thus, the cultural and spiritual beliefs of the community need to be taken into account before providing the services and care for the health of the Mãori, according to their beliefs and traditions. Colonization and other contexts can affect the health outcomes of the people in the Mãori community. These factors can influence the inequity in the healthcare services and thus be responsible for its complexity and the way in which the choices of the patients were affected (Stuff 2020).
Hence, the traditions and beliefs of the Mãori community can affect the decisions that the health professionals take for the care and services that they provide to the patients that they have.
Conclusion
In conclusion, the healthcare providers would need to have a holistic approach towards protecting the interests of the Mãori patients that they have regarding the various aspects of the services like the physical, emotional, financial and other aspects of the patients and their families when they are threatened by life-threatening illnesses so that palliative care can be advanced, with better quality of life for the patients.
References
Altilio, T., Otis?Green, S., Hedlund, S., & Fineberg, I. C. (2019). Pain management and palliative care. Handbook of health social work, 535-568.
https://doi.org/10.1002/9781119420743.ch22
Asadzandi, M. (2018). Spiritual empowerment program based on sound heart model in the cancerous children’s family. Annals of Nursing Research and Practice, 3(1), 1026. http://ishcc.ir/uploads/Spiritual%20Empowerment%20Program%20%20(157u).pdf
Astrow, A. B., Kwok, G., Sharma, R. K., Fromer, N., & Sulmasy, D. P. (2018). Spiritual needs and perception of quality of care and satisfaction with care in hematology/medical oncology patients: a multicultural assessment. Journal of Pain and symptom management, 55(1), 56-64. https://doi.org/10.1016/j.jpainsymman.2017.08.009
Baillie, J., Anagnostou, D., Sivell, S., Van Godwin, J., Byrne, A., & Nelson, A. (2018). Symptom management, nutrition and hydration at end-of-life: a qualitative exploration of patients’, carers’ and health professionals’ experiences and further research questions. BMC palliative care, 17(1), 1-13. https://doi.org/10.1186/s12904-018-0314-4
Best Practice Advocacy Centre New Zealand. (2022). Practical solutions for improving M?ori health, Retrieved 12 February 2022 from < https://bpac.org.nz/bpj/2008/may/docs/bpj13_solutions_pages_10-14.pdf>
Brooks, C., Ballinger, C., Nutbeam, D., Mander, C., & Adams, J. (2020). Nursing and allied health professionals’ views about using health literacy screening tools and a universal precautions approach to communication with older adults: a qualitative study. Disability and rehabilitation, 42(13), 1819-1825. https://doi.org/10.1080/09638288.2018.1538392
Capital & Coast District Health Board. (2022). Tikanga M?ori, Retrieved 12 February 2022 from
Conversano, C. (2019). Common psychological factors in chronic diseases. Frontiers in Psychology, 10, 2727. https://doi.org/10.3389/fpsyg.2019.02727
Damanik, S. R. H., & Chen, H. M. (2021). Family needs among patients hospitalized in critical care unit: Scoping review. Enfermería Clínica, 31, 541-548. https://doi.org/10.1016/j.enfcli.2021.09.001
Dißmann, P. D., Maignan, M., Cloves, P. D., Gutierrez Parres, B., Dickerson, S., & Eberhardt, A. (2018). A review of the burden of trauma pain in emergency settings in Europe. Pain and therapy, 7(2), 179-192. https://doi.org/10.1007/s40122-018-0101-1
Etkind, S. N., Bone, A. E., Gomes, B., Lovell, N., Evans, C. J., Higginson, I. J., & Murtagh, F. E. M. (2017). How many people will need palliative care in 2040? Past trends, future projections and implications for services. BMC medicine, 15(1), 1-10. https://doi.org/10.1186/s12916-017-0860-2
Gao, Y., Wei, Y., Yang, W., Jiang, L., Li, X., Ding, J., & Ding, G. (2019). The effectiveness of music therapy for terminally ill patients: a meta-analysis and systematic review. Health care assignment Journal of pain and symptom management, 57(2), 319-329. https://doi.org/10.1016/j.jpainsymman.2018.10.504
Greenberg, J. A., Basapur, S., Quinn, T. V., Bulger, J. L., Schwartz, N. H., Oh, S. K., ... & Glover, C. M. (2021). Challenges faced by families of critically ill patients during the first wave of the COVID-19 pandemic. Patient education and counselling, 105(2), 297-303. https://doi.org/10.1016/j.pec.2021.08.029
Hahn, S.M. (2020). The Critical Role of Health Care Professionals During the COVID-19 Pandemic, Retrieved 12 February 2022 from < https://www.fda.gov/news-events/speeches-fda-officials/critical-role-health-care-professionals-during-covid-19-pandemic-08102020 >
Keramatikerman, M. (2020). A Systematic Review on Challenges Faced by Family Caregivers of Cancer Patients., Open Access Journal of Biomedical Science, 2(4). https://dx.doi.org/10.38125/OAJBS.000191
Ming, Y., Wei, H., Cheng, H., Ming, J., & Beck, M. (2019). Analyzing patients' complaints: awakening of the ethic of belonging. Advances in Nursing Science, 42(4), 278-288. 10.1097/ANS.0000000000000278
Mitchell, G. K., Senior, H. E., Johnson, C. E., Fallon-Ferguson, J., Williams, B., Monterosso, L., ... & Yates, P. M. (2018). Systematic review of general practice end-of-life symptom control. BMJ supportive & palliative care, 8(4), 411-420. http://dx.doi.org/10.1136/bmjspcare-2017-001374
Mithrason, A. T., & Parasuraman, G. (2017). Physical problems and needs of patients in palliative care center. International Journal of Community Medicine and Public Health, 4(11), 4145. http://dx.doi.org/10.18203/2394-6040.ijcmph20174818
Rosmarin, D. H., Salcone, S., Harper, D., & Forester, B. P. (2019). Spiritual psychotherapy for inpatient, residential, and intensive treatment. American Journal of Psychotherapy, 72(3), 75-83. https://doi.org/10.1176/appi.psychotherapy.20180046
Ruth-Sahd, L. A., Hauck, C. B., & Sahd-Brown, K. E. (2018). Collaborating with hospital chaplains to meet the spiritual needs of critical care patients. Dimensions of Critical Care Nursing, 37(1), 18-25. 10.1097/DCC.0000000000000279
Shahin, W., Kennedy, G. A., & Stupans, I. (2019). The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: a systematic review. Patient preference and adherence, 13, 1019. https://dx.doi.org/10.2147%2FPPA.S212046
Stuff. (2020). Health care providers should consider practices, values and beliefs in wh?nau M?ori care, report says. Retrieved 12 February 2022 from
Tong, S. T., Liaw, W. R., Kashiri, P. L., Pecsok, J., Rozman, J., Bazemore, A. W., & Krist, A. H. (2018). Clinician experiences with screening for social needs in primary care. The Journal of the American Board of Family Medicine, 31(3), 351-363. https://doi.org/10.3122/jabfm.2018.03.170419












