Health Care Assignment: System Thinking for Improving Health Care Services
Question
Task: This assessment includes a high quality written health care assignment on the insights offered by system thinking.
First, pick a public health problem or a health services management problem of your choice that you think would benefit from systems analysis or systems thinking. Part 1 of the assessment requires you to briefly review any existing evidence that has adopted a systems approach to better understand or address your problem. Part 2 requires you to describe that method or methods you would use to shed further light on the problem or its possible solutions.
Answer
Introduction
Public Health Issues have been an increasing trend in many countries of the world. The public health care systems are still not developed and aligned with technological tools and systems that will eventually improve public health domains. There are different strata of the society that consists of varied income classes who cannot afford expensive health care services;thus, they look to the health services provided by different agencies which are funded by the government and non- profit organizations. The report will aim in conducting a literature review on public health issues along with the justification methods and process.
This assignment relates to the application of system methods in public health domain for maintaining the physical records of patients. Increasing population along with various disease has complexed maintenance of physical medical records that increases the cost of health care units while also impacts the patient outcomes. In this view, Electronic Health Records is a digital solution to recording the medical history of the patients.EHR is an automated process that helps in accessing information and improves the workflow of the clinic. It also supports the activities that are directly or indirectly related to care via different interfaces like evidence-based decisions, managing quality, and outcomes (Seymour et al, 2012).
Part 1- Literature Review
Application of System Methods
The public health care systems are complexed that are made of heterogeneous elements. Public health domains have started to use system sciences in the pandemic for shaping practices and policies. However, system science studies and other analytic methods remain underutilized while they are not featured in the curriculum and training in public health. Luke & Stamatakis (2012) suggested that system science includes system dynamics, network analysis, and agent-based modeling. Luke & Stamatakis (2012) depicted that system method are translational and are commonly explicit in the real-time models. Thus, the growing demand for system methods will account for greater complexity. The system science methods for public health are advantageous but the system methods are often underutilized and lack visibility.Carey et al (2015) investigated the methodologies that are being in public health domains while identifying fruitful activities. The author had conducted 117 articles that are included in the review of qualitative controls. System sciencestrengthens public health efforts thus also revealing restrictions about the dynamic systems. The author suggests soft systems modelling techniques will be most useful in the public health domain.
Kohli & Tan (2016)opined that in the past two decades, EHR technology is developing at a faster rate and is equipped with essential functionalities. The improved functionalities are contributed by advancement in the technology and demand by the customers for incorporating several features that have resulted in efficiency and high-quality care. However, there is no evidence that EHR is the best fit for solving issues of data management.
In a study by Wanjau et al (2012). It was depicted that factors on service quality were explored in the Public Health Sector in Kenya. The author had conducted a study on 103 respondents in Central & Eastern Africa of results indicated that low employee capacity, ineffective technology adoption, and ineffective communication channels had impacted the overall services delivery in the public health domains. The author suggested that the implications for improving public health policy will include comprehensive health care policies, improved working conditions, improved system methods for high service qualities. Maina et al, (2019) opined that Geographic Information Systems encouraged refined metrics for health care access. The author opined access to health care has been complexed referring to geographic availability. The application of systemmethods will help in defining the inequalities of the provision of the services and informed planning. The spatial health access will require information about the providers along with their locations.
Furukawa et al, (2014) opined that the US has been making substantial investments in accelerating the adoption and usage of EHR in the public health care domain. The author conducted a study and found a significant gap in the usage of HER in solo- practices and primary health care thus, only 78% of the office-based practitioners had accepted EHR while 48 % were capable of incorporating the EHR systems. Furukawa et al, (2014) further defined that 14% of the patient data was being shared with the external providers while 34 % used system messaging services for interacting with patients, and 25% of practitioners were involved in online patient care. It can be said that EHR systems can in a developing stage and will provide substantial benefits to the caregivers and receivers. The government should play an active role in growing the adoption of EHR, information sharing, and engaging the patients.
De Pietro & Francetic (2018) further demonstrated that the e-health strategywas launched in the year 2015 in which Switzerland had passed federal law regarding the Electronic Health Record. Thus, the reform required the patients for adopting interoperable EHRs for facilitating data sharing and cooperation amongst the health care units, thus improving the care quality. In this view, security issues should be one of the major concerns for software designers of EHR. Despite establishing Federal law, the Swiss health care systems lack stakeholder agreements due to which the processes of electronic health record systems have slowed down. It is very essential for putting proper incentives in place for technical implementation and proper management of HER and other system methods. Rea et al, (2012) depicted that Strategic Health IT Advanced Research Projects (SHARP) was established by the National Co-Ordinator of Health Information Technology. The improvising done by SHARP would encourage the use of Electronic Health Records for care processes, improving outcomes, biomedical researches, and national supervision. However, the author suggested that this system will encounter informatic problems for standardizing disparate health information from national health care firms and providers.
Singh et al, (2013), studied physician-level variations for using the electronic health records features that were associated with other factors. The author had used a cohort study and commercial database from the year 2010 to 2013 for determining the early usage of EHR in the organization. Thus, it was estimated that practitioner level usage of Electronic Health Records can be an additional predictor for reducing costs and health care quality.Sittig & Singh (2012) proposed that three-phase frameworks for developing EHR patient safety. Thus, the first phase of the framework aims at goals for mitigating risks that should be unique and specific with the technology. The second phase framework should address the failures of technology for supervising health care while the final phase will detect potential issues in patient safety for using electronic data record systems. The literature review suggested the inefficiencies of electronic health records in a different system in different countries thereby research is ongoing for rolling out this strategy from a broader perspective.
Part 2- Application & Implementation
Application and Implementation of System Thinking
Applying systems thinking method this problem can easily be tackled. As depicted by Bates et al, (2014) the health care systems of US health systems have been adopting the health care records for improving the availability of clinical data. Rapid progress in clinical analytics has been done through the evaluation of voluminous data through Big data analysis. The author depicts that the use of Big Data has unprecedented opportunities that might reduce the average costs of public health care domains. For clinical analytics data like algorithms, registries, assessment scores, and others shall be implemented by the organizations for reducing costs and improving care, however, privacy concerns and research analytics are one of the major issues of applying system methods in health care. In another study by Springate et al, (2014) it was reported that clinical code is one of the major foundations in research undertaken for electronic medical records. If the lists of the clinical codes are not present, it becomes difficult for reviewers for determining theresearch validity. The author has built an online repository that can be used for uploading and downloading medical records.
Causal Loop Diagram
The health care systems of several countries lack proper maintenance of health records of different patients. As the population is increasing, the health care units are required a high level of maintenance systems for retrieving data about the patient for diagnosing and prescribing appropriate treatment and medications. Operating on digital mediums is important as there is a high risk of losing or misplacing the physical records. Lack of proper Health Records often leads to an increased financial burden on the patients as they are required to conduct repeated health tests for diagnosing the issue. Also, the previous records are helpful for practitioners for obtaining insights about the previous health issues and treatments the patients have undergone through which correct diagnosis of the current problem can be done. Large physical patient data secure space and time when information is needed on an urgent basis. The implementation of Electronic Health Records might solve this issue and strengthen health care systems.
The health care systems in Australia have been facing a huge crisis in maintaining the physical records of the patients. The influx of patients has been increasing due to which retrieving data is nearly impossible. The issue increases when the patients are admitted in emergencies, the carers of the patients have to huge documents which are challenging for the doctors to analyse and start the treatments. The disease influx has also been increasing due to data management has become cumbersome.
The Causal Loop Diagram helps in analysing contexts of all issues. About system methods, the causal loop diagrams have depicted concerns of privacy issues in the current systems. Many countries have been facing issues for implementing system methods like data analytics and EMR due to complicated public health policies and privacy concerns (which is also depicted in the diagram).
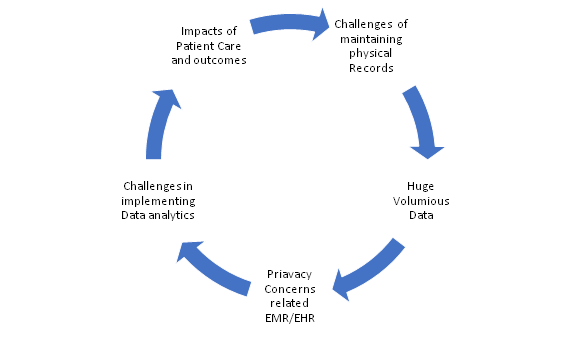
Figure 1:Author's Creation
Potential Outcomes From EHR
The Electronic Health/ Record Management systems are adopted by several governments for reaching goals line improvement in quality care, managing chronic disease, feasibility, and efficacy. The EHR systems perform various functions that are
- Providing Health Information– The electronic record systems collect several clinical data that includes diagnoses, allergies, medications, and many others. It not only collects the vital information but also processes and stores the information in a way that is easily accessible, transmitted, and evaluated by the health care staff.
- Managing Results- The practitioners are encouraged to provide quality care as these digital systems encourage the care providers to access the new and past medical history of the patients. If the patients are required to refer to other organizations, these data can be easily transferred thereby co-ordinating in quality care by correct treatment and diagnosis (Seymour et al, 2012). This also reduced the costs of storing physical data by the organizations and the patients.
- Managing Orders- Quality Patient care is one of the important aspects in multiple settings of the health care units. Thus, the digital record systems will encourage the clinicians for managing the store orders, prescriptions, and others for enhancing the legibility, reducing duplication while improving the speed of executing the orders (Tao et al, 2012).
- Supporting Decisions– The notifications and decision support will improve the clinical compliances, also ensure frequent screenings and other preventive measures (Sittig & Wright, 2015). The decision support systems are not only helpful in enhancing the clinical decisions but it also improves the health of the population by reminding them to preventive measures to be undertaken for mitigating chronic disease risk and complying with treatment plans prescribed by the doctor.
- Providing platforms for communication and connectivity– The care- coordination and patient engagement are enhanced by accessing messaging applications that provide a platform for sending and receiving communication amongst the care providers and receivers.
- Supporting Patients- The Patient Support Tools helps the individuals in accessing their medical records and educating them through appropriate materials. In cases of home- monitoring for patients suffering from chronic ailments, the health care providers will be assisted by digital tools thereby helping the patients in improving chronic conditions through self-management and self-testing (Daniel et al, 2014).
- Administrative Procedures- The procedures and reporting standards of healthcare units belong to the administrative functions. The electronic health records systems ease the scheduling process, improves efficiency while also provides timely services to all the patients. Thus, receiving on-time care, the financial burden from high costs treatments is reduced from the health budget of patients.
- Reporting Standards: For improving community health, electronic Health Records are capable of storing and transmitting information about safety and surveillance of disease. The report and population health functionality will be able to build the practice of submitting the immunizations data while also receiving forecasts from the public health history of immunizations (Jensen et al, 2012). This will be very helpful for protecting the children from various chronic diseases as they can be provided booster doses and immunity vaccines based on their immunization history. If the systems are appropriately adopted by the public and private health care units, the organizations will experience cost reduction procedures with efficient management of quality patient care. The health care staff should be encouraged through proper rewards and recognition systems for implementing digitisation in the health care management process.
Justification of the methods Proposed
Electronic health record systems are beneficial for public health systems as all individuals will be eligible for equivalent healthcare without increasing the financial burden of treatment on the individual. It is often seen that private health care units have advanced equipment and processes that can ensure high-quality care. However, in middle and low- income earning countries, the population is huge while income is distributed unevenly amongst the citizens. The public health sector is weakened with low infrastructure and high demand from the population. In such scenarios, straightening the public health care domains are important for catering to the huge health care demands. The use of electronic mediums and strengthening public health systems is one-time investment costs for the government and qualityhealth care can be accessed by the larger population (Sun et al, 2015). On the contrary, the developed economies face a different set of issues in implementing quality standards. The first part of this report condemned the literature review and it was established that many countries have not completely successful in incorporating electronic health records. The government and stakeholders should realize the profitability of the advanced systems and work in collaboration to ensure safe and secure systems are established for rendering high patient care.
The secured EHR systems might enable the practitioners to share patient information with other health care units and authorized dignitaries for improving patient care. It will also facilitate active communication amongst the health care workers thereby enabling information integration and patient care- coordination. The system-based reminders will help the patients and the practitioner for improving compliance with protective service protocols. Biomedical informatics has improved the health care systems thereby using surveillance and inquiry facilities in a digitally stored system (Lawanyashri et al, 2017). The inquiry systems of Electronic Health Records will help in detecting the criteria of patients for clinical trials. The surveillance facilities of these systems will help in supporting the clinical trials by keeping the track of patient visits and succeeding in different phases of the experiments as per protocols. The research in the clinical research will be executed by extracting the routine medical records thus costs and time of research on collecting the data manually from the patient's medical records.
Conclusion
The health care systems of several countries lack proper maintenance of health records of different patients thus, as the population is increasing, the health care units are also required a high level of maintenance systems for retrieving data about the patients. This will help in correctly diagnosing and prescribing treatment and medications to several sets of patient’s bases. Electronic Health Records is a digital solution to recording the medical history of the patients. It is generally maintained by the health care provider or by Government to provide high-quality patient care. These systems are capable of providing detailed insights of the patients about their issues, prescribed medicines, demographic structure, radiology reports, past medical history, vaccinations & immunizations, and many others. The implementation of the EHR can only be done through a high commitment from the stakeholders and medical officials.
References
Bates, D. W., Saria, S., Ohno-Machado, L., Shah, A., & Escobar, G. (2014). Big data in health care: using analytics to identify and manage high-risk and high-cost patients. Health Affairs, 33(7), 1123-1131.
Carey, G., Malbon, E., Carey, N., Joyce, A., Crammond, B., & Carey, A. (2015). Systems science and systems thinking for public health: a systematic review of the field. BMJ open, 5(12).
Daniel, C., Sinaci, A., Orange, D., Sadou, E., Declerck, G., Kalra, D., ... & Hussain, S. (2014).
Standard-based EHR-enabled applications for clinical research and patient safety: CDISC–IHE QRPH–EHR4CR & SALUS collaboration. AMIA Summits on Translational Science Proceedings, 2014, 19.
De Pietro, C., & Francetic, I. (2018). E-health in Switzerland: The laborious adoption of the federal law on electronic health records (EHR) and health information exchange (HIE) networks. Health Policy, 122(2), 69-74.
Furukawa, M. F., King, J., Patel, V., Hsiao, C. J., Adler-Milstein, J., & Jha, A. K. (2014). Despite substantial progress in EHR adoption, health information exchange and patient engagement remain low in office settings. Health Affairs, 33(9), 1672-1679.
Jensen, P. B., Jensen, L. J., & Brunak, S. (2012). Mining electronic health records: towards better research applications and clinical care. Nature Reviews Genetics, 13(6), 395-405.
Kohli, R., & Tan, S. S. L. (2016). Electronic health records: how can IS researchers contribute to transforming healthcare?. Mis Quarterly, 40(3), 553-573.
Lawanyashri, M., Balusamy, B., & Subha, S. (2017). Energy-aware hybrid fruitfly optimization for load balancing in cloud environments for EHR applications. Informatics in Medicine Unlocked, 8, 42-50.
Luke, D. A., & Stamatakis, K. A. (2012). Systems science methods in public health: dynamics, networks, and agents. Annual review of public health, 33, 357-376.
Maina, J., Ouma, P. O., Macharia, P. M., Alegana, V. A., Mitto, B., Fall, I. S., ... & Okiro, E. A. (2019). A spatial database of health facilities managed by the public health sector in sub Saharan Africa. Scientific data, 6(1), 1-8.
Rea, S., Pathak, J., Savova, G., Oniki, T. A., Westberg, L., Beebe, C. E., ... & Chute, C. G. (2012). Building a robust, scalable, and standards-driven infrastructure for secondary use of EHR data: the SHARPn project. Journal of biomedical informatics, 45(4), 763-771.
Seymour, T., Frantsvog, D., & Graeber, T. (2012labour-intensive records (EHR). American Journal of Health Sciences (AJHS), 3(3), 201-210.
Singh, H., Spitzmueller, C., Petersen, N. J., Sawhney, M. K., Smith, M. W., Murphy, D. R., ... & Sittig, D. F. (2013). Primary care practitioners' views on test result management in EHR-enabled health systems: a national survey. Journal of the American Medical Informatics Association, 20(4), 727-735.
Sittig, D. F., & Singh, H. (2012). Electronic health records and national patient-safety goals. The New England journal of medicine, 367(19), 1854.
Sittig, D. F., & Wright, A. (2015). What makes an EHR “open” or interoperable?. Journal of the American Medical Informatics Association, 22(5), 1099-1101.
Springate, D. A., Kontopantelis, E., Ashcroft, D. M., Olier, I., Parisi, R., Chamapiwa, E., & Reeves, D. (2014). ClinicalCodes: an online clinical codes repository to improve the validity and reproducibility of research using electronic medical records. PloS one, 9(6), e99825.
Sun, H., Depraetere, K., De Roo, J., Mels, G., De Vloed, B., Twagirumukiza, M., & Colaert, D. (2015). Semantic processing of EHR data for clinical research. Journal of biomedical informatics, 58, 247-259.
Tao, C., Wongsuphasawat, K., Clark, K., Plaisant, C., Shneiderman, B., & Chute, C. G. (2012, January). Towards event sequence representation, reasoning, and visualization for EHR data. In Proceedings of the 2nd ACM SIGHIT International Health Informatics Symposium (pp. 801-806).
Wanjau, K. N., Muiruri, B. W., & Ayodo, E. (2012). Factors affecting the provision of service quality in the public health sector: A case of Kenyatta national hospital.












