Operations Management Assignment: Case Analysis On Pre-Admission Testing Area Of Massachusetts General Hospital
Question
Task:
Read the case study of Massachusetts General Hospital's Pre-Admission Testing Area (PATA) by Kelsey McCarty, Jérémie Gallien, Retsef Levi and prepare an operations management assignment answering the following 3 questions:
- What is the perspective of the key stakeholders involved in PATA´s current operational performance?
- Draw a process flow diagram of the PATA patient visit process. Calculate the capacity and utilization rate for each key resource involved. Where is the clinic’s bottleneck?
- Indicate 3 changes you would recommend to improve the PATA patient visit process. Explain what you expect from these changes.
Answer
1.0 Perspectives of the key stakeholders of the hospital discussed in the operations management assignment:
Because of substantial advances in study and equipment, the danger of providing anesthesia has dropped dramatically from the beginning of the 1990s. Nevertheless, there were still dangers, and problems might lead to lifelong impairment or deaths. Surgeons wanted to understand ahead of time if a person's body was capable of withstanding anesthesia. As a result, every surgical sufferer became obliged to have a "pre-admission work-up." The PATA center was in charge of performing the required for every outpatient, accounting for 43percent of all surgery admissions.
1.1 Nurse and medicine doctors:
Certified nurses and medical physicians generally paid on the basis of working from 7:00 a.m. until 5:00 p.m. daily; nevertheless, consultations were seldom finished by this same hour. Waiting beyond 6:00 p.m. was becoming standard, and doctors often were seen as late as 7:00 p.m. or possibly 8:00 p.m. Anxiety was rising as the number of patients in the waiting area grew and the hours became longer (Vergara et al., 2017).
1.2 Surgeons:
Surgeons have been the only group of people afflicted by the PATA issues. They assessed the person's health problem and the sort of operation that has been required. They have been also in charge of scheduling their sufferers' PATA visits, which had to be arranged between Thirty days following the procedure. Due to the obvious restricted capability, it became widely agreed that the greatest complicated instances would be given precedence. Nevertheless, the situations that came under this group were not properly delineated. Because of the absence of defined criteria and the diversity in surgeon diagnoses, critical patients were frequently not referred to PATA whereas adolescent and healthier patients did.
1.3 OR directors and other medical heads:
According to Zalboni et al. (2020), a plan was brought up by the OR directors and other medical executives to construct a second PATA center. The Mass General West subsidiary campus in Waltham, Massachusetts, had availability, and industry analysis indicated that this could be the chosen destination for a substantial number of PATA clients. Establishing a secondary center here will allow the facility to treat 100% of surgery patients while also allowing it to experiment with novel practice models while upsetting the MGH atmosphere. Notwithstanding the strength of the offer, PATA had been an expense centre, and the MG West location was eventually assigned to a further (profit-generating) division at MGH that had also requested the location.
Notwithstanding the operational performances, PATA provided excellent service and was particularly concerned about healthcare reliability. Despite the constraints of decentralization, lengthy wait hours, OR difficulties, and angry clients and doctors, it might have been simple to cut corners, but the MGH team stayed dedicated to complete pre-admission work-ups to guarantee a successful and uncomplicated operation. That was the main motto and whole perspective of the PATA stakeholders.
2.1 Flow Diagram of PATA patient visit process:
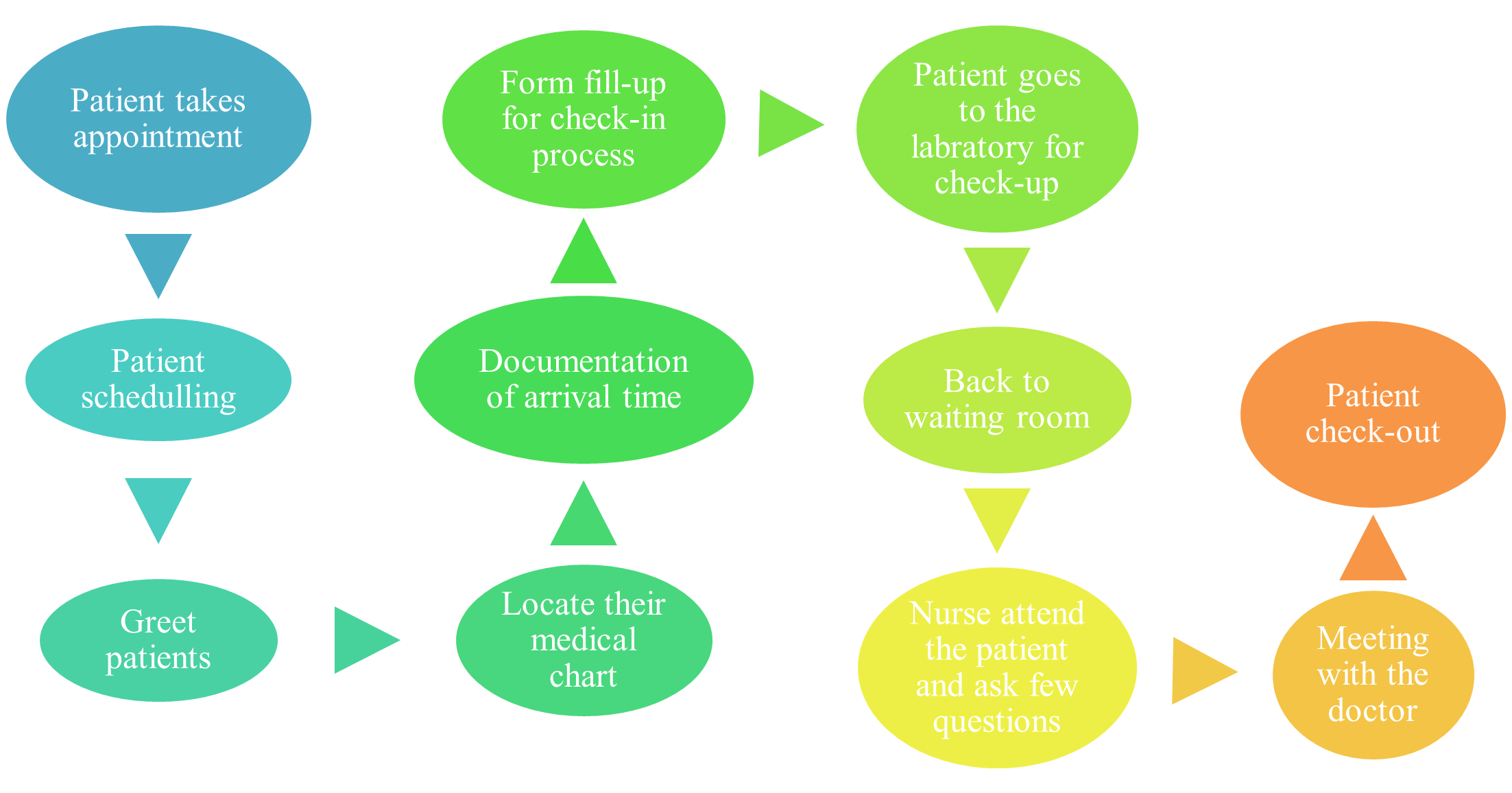
Figure 1: patient visit process
(Source: Self-created)
2.2 Calculation of the capacity and utilization rate:
Capacity= Arrival rate of patient (?)
Normal, (?) = four patient/ half an hour = eight patient per hour
Launch, (?) = two patient/ half an hour = four patient per hour
Average, (?) = fifty-six patient / eight hours = seven patient per hour
Capacity of nurse, whilst launch = 2RN * forty three minutes = 2.8 patient per hour
Capacity of nurse, whilst normal = 5RN * forty three minutes = seven patient per hour
Utilization rate = (actual output/potential output)*100 = (55/65)*100= 84.615%
2.3 Bottleneck of the Clinic:
The accusation nurse's roster is useful for monitoring patients, chambers, and doctors, although it has numerous flaws. Whenever a nurse or doctor forgets to enter their names upon that chart, two doctors may believe they are treating the similar person. In other cases, names were put in yet the provider was unaware that they had been chosen. The former situation resulted in duplication and the wastage of prior doctor effort; the other situation resulted in patients staying up to half an hour longer.
Additional issue is that the process is dependent on physicians notifying the lead nurse whenever they are present. If there are no people waiting to be treated, doctors will frequently depart to complete other tasks or take a rest. Once a patient becomes accessible, the lead nurse has to vacate their unit to locate a doctor who is obtainable. This lengthened the duration patients waited and, on occasion, caused the head nurse to overlook critical patient circulation incidents while being absent at the unit (Verger et al., 2017).
A further major flaw in the entire PATA procedure is that people have been known to leave in the midst of appointments because they are weary of waiting. Several of the causes people occasionally showed up for operation with unfinished PATA documents were because of this. Quite frequently than not, work-ups remained unresolved since doctor teams failed to send PATA doctors the health information they required to conduct their evaluations. If the documentation were delivered whatsoever, it typically took many phone conversations, making doctors irritated by their overall loss of oversight over the procedure.
3.0 Recommendations for three changes:
- Previously, Monday through Friday, from 7:00 a.m. to 5:00 p.m., the hospital was open. Due to any person's medical condition, the time frame must be extended. Previously, four patients were scheduled per 1/2 hour from 7:00 a.m. to 3:00 p.m., other than between lunch breaks, while only 2 people were assigned. This procedure must also be altered in order to reduce the patient's waiting time. Each half hour, the physicians must diagnose at least six to seven patients. The consultations must be handled using MGH equipment that permits doctors' teams to register in and organize people for PATA visits. This will allow the providers to sustain their good will and every critical patient also will be satisfied by the process. As the waiting time will be reduced, the tension between the patient party and doctors will also be decreased. More doctors need to be activated at the same time so that the process can get some pace. This will also reduce the mortality rate in the hospital.
- Before, the research lab was divided under two offerings: 1) two units for taking outpatient vital signs and EKGs at the start of the visit, and 2) 3 units for taking client blood specimens at the conclusion. To reduce a person's waiting time, these unit services should be expanded. Because doctors require vitals and an EKG to assess a patient's condition, this procedure must be completed initially. Anesthetists should count each patient and apply changes to the usual medical tests report types depending on the assessment results. Blood tests must be performed at the conclusion of the session to avoid spreading infectious illness through a syringe. Per day, 5 laboratory personnel were assigned, individually qualified to operate at either unit. Because of the busy patient schedule, more lab workers must be activated at the same time. The process will gain speed as more personnel operate in accordance with it. In Laboratory more EKG mechanisms need to be placed so that technicians can diagnose more patients at a time, which will eventually reduce the waiting time and they also can prioritize critical patients even in the busy schedule. It will eventually lower the anger of the patient party and the mortality rate also be reduced.
- Over 5 laboratory techs, 5 nursing staff, and 8 anesthetists should be scheduled every day by the PATA medical coordinator. The nurses will collaborate to execute a unified clinical evaluation document for more individuals, which will speed up the procedure. At the same time, the anesthetists will examine the person's complete condition and acquire the authorization from the person for anesthesia.
Using what they'd observed from previous initiatives, the working group concentrated solely on remedies that will necessitate organizational PATA modifications. They investigated enhancing triaging, 7 giving patient information regarding what to anticipate at the date of operation through the internet instead of in-clinic, and moving from papers to computerized health files. Nevertheless, putting these concepts into action will necessitate extra cash, staff, and infrastructure. Furthermore, while the working group recognizes that all of these measures will undoubtedly assist, the response team will also note that they would not address the primary root of PATA's issues. Notwithstanding such setbacks, the task team kept brainstorming new methods to enhance PATA. These changes will heavily impact on the reputation of the hospital. It will strengthen the trust of the patient towards the hospital. These facilities will also improve the look after procedures. The patients will avail a quality treatment and it will eventually escalate the good will of the hospital. Behavior of the providers and the fast paced process will also attract other patients to visit the hospital for quality treatment.
Reference List
Vergara, J.C., Woodmansee, M.L., David, L. and McClurkin, S., (2017). “We Hear You” Changing the Culture of Caring, One Patient at a Time. Journal of PeriAnesthesia Nursing, 32(4), pp.e14-e15. Available at: https://www.jopan.org/article/S1089-9472(17)30209-5/abstract [Assessed on 1st october, 2021]
Zaniboni, A., Ghidini, M., Grossi, F., Indini, A., Trevisan, F., Iaculli, A., Dottorini, L., Moleri, G., Russo, A., Vavassori, I. and Brevi, A., (2020). A review of clinical practice guidelines and treatment recommendations for cancer care in the COVID-19 pandemic. Operations management assignment Cancers, 12(9), p.2452. Available at: https://www.mdpi.com/2072-6694/12/9/2452/pdf [Assessed on 1st october, 2021]












